Differences between Indicator 15 (Intrapartum stillbirth and very early neonatal death rate) & Indicator 16 (Neonatal inpatient mortality rate)
Stillbirths and newborn mortality in health facilities
Stillbirths and newborn deaths can be separated into different categories (Table 1).
Table 1: Categories of stillbirths and newborn deaths1
| Term | Definition |
|---|---|
| Stillbirth | A baby born following a fetal death at 154 days (22+0 weeks) or more of gestation |
| Late gestation stillbirth* | A stillbirth at 196 or more days gestation (≥28+0 weeks) |
| In-facility stillbirth | A stillborn baby who was known to be alive at admission |
| Antepartum fetal death | A fetal death before the onset of labour or the birthing process |
| Antepartum stillbirth | A stillbirth following antepartum fetal death |
| Intrapartum fetal death | A fetal death during labour or the birthing process |
| Intrapartum stillbirth | A stillbirth following intrapartum fetal death |
| Neonatal death | A death during the first 28 completed days after a live birth (0-27 days) |
| Early neonatal death | A death during the first 7 completed days after a live birth (0-6 days) |
| Very early neonatal death | A death during the first 24 hours after a live birth (0-24 hours) |
* Used for international comparisons for the purpose of global estimates
Indicators 15 & 16
The EmONC Framework includes two facility-based indicators that can be used to measure changes in stillbirths and newborn mortality (Table 2). The two indicators measure different types of stillbirths and newborn deaths and have different purposes.
Table 2: EmONC indicators measuring impact on stillbirths and newborn mortality in health facilities
| Indicator | Type(s) of stillbirths and newborn deaths | Purpose |
|---|---|---|
| Indicator 15: Intrapartum stillbirth and very early neonatal death rate | In-facility intrapartum stillbirths and very early neonatal deaths | Assesses the quality of intrapartum and immediate postnatal care. |
| Indicator 16: Neonatal inpatient mortality rate | Deaths among newborns receiving inpatient care | Provides an overall picture of whether inpatient care provided to small and sick newborns is effective in reducing mortality. |
Although the purposes of these two indicators are different, there is not a clean division in the neonatal deaths included in their calculation (i.e., neonatal deaths that occur in an inpatient newborn care unit within the first 24 hours after birth may be included in both indicators).
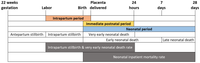
Figure 1: Timeline showing which periods of care and deaths are captured by the EmONC indicators measuring impact on stillbirths and newborn mortality in health facilities
While the purpose of Indicator 16 is to give an indication of the quality of inpatient care for small and sick newborns, the death of an inpatient newborn in the first 24 hours after birth may actually come as a result of poor intrapartum care rather than poor inpatient care. Though it may not be possible to determine the most important contributing factors for all deaths included in either indicator, these indicators can still be useful for flagging issues with EmONC service delivery in different units in health facilities.
Blencowe H, Okwaraji Y, Hug L, You D. Stillbirth Definition and Data Quality Assessment for Health Management Information Systems (HMIS), a guideline. 2022 (accessed 2023 December 22). ↩︎